What is the potential cost of not having Bariatric Surgery?
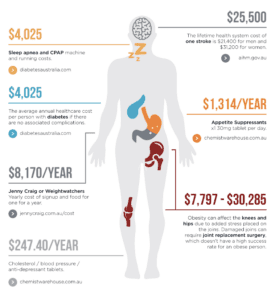
Bariatric/weight loss surgery does come with a large price tag and for a lot of patients the figure can be very discouraging. A fundamental area that is not often thought about is what the potential cost of not having the surgery could be on you and our health care system.
Fear of the social stigma, fear of failing and the cost involved of bariatric surgery, have been just a few other reasons why so many have stuck to more conventional weight loss strategies and are reluctant to have the surgery. Nevertheless, the popularity of bariatric surgery is becoming increasingly popular with patients choosing this ‘tool’ centered option to help with weight loss and long term maintenance.
With the tripling of incidence since 1975, the World Health Organisation estimates that most of the world’s population now live in countries where being overweight and obese kills more people than being underweight.
The Australian Burden of Disease Study highlights obesity as the second largest risk for fatal disease and largest risk for non‐fatal disease over the past 15 years. While death rates have been mitigated by a 35% increase in cardiovascular medicine prescriptions and a doubling of diabetes management therapies, our ability to successfully maintain this approach is likely to be overrun as Australian obesity rates climb to over 40% within a decade.
Aside from the individual health impact, obesity creates significant community cost implications — direct costs are estimated to be $5.4 billion and indirect costs a further $6.4 billion per year in Australia.
Let’s look at the disease risk of obesity.
Bariatric surgery, however, remains the most durable and effective treatment for obesity, achieving in most patients 20–30% total body weight loss (TBWL) for up to 20 years after surgery and improving comorbidities and quality of life. Randomised trials have demonstrated bariatric surgery to be superior in the treatment and control of type 2 diabetes compared with medical management, and improvements in sleep apnoea, high blood pressure, metabolic syndrome, polycystic ovary syndrome, non‐alcoholic steatohepatitis and arthritic disease have been extensively documented. Most compellingly, matched cohort studies have demonstrated clear reduction in all‐cause mortality for patients with obesity undergoing bariatric surgery, with particular decrease in cardiovascular and cancer death compared with their non‐operated cohorts. These health benefits translate to substantial health care cost savings, the magnitude of which is equivalent to smoking cessation.
Savings in the long term
Yes, it is true that the decision to have bariatric/weight loss surgery will mean spending more money on items such as new clothing, dietary supplements, fitness and check-up appointments, but you will see significant savings are gained in your food bill, medication and medical bills.
In conclusion, bariatric surgery pays off in the long-term, financially, physically, mentally and reduces the burden on our already overloaded health care system.
World Health Organisation. Obesity and overweight 9 June 2021. https://www.who.Int/news/fact-sheets/detail/obesity-and-overweight (viewed May 2023).
Australian Institute of Health and Welfare. Australian Burden of Disease Study: Impact and causes of illness and death in Australia 2018) Australian burden of Disease Study Series No. 23; Cat. No. Bod 29.) Canberra: AIHW 2021. https://www.alhw.gov.au/getmedia/5ef18dc9-414f-4899-bb35-08e239417694/alhw-bod-20.pdf.aspx?inline+true (viewed May 2023)
Cleslik LK, Cresswell NR, Fineberg, D, et al. Prescription trends and costs of diabetes medications in Australia between 2003 and 2019: an analysis and review of the literature. Intern Med J2020; 52:841-847
Ahmad Aly, Michael L Talbot and Wendy A Brown Med J Aust 2022; 217 (5): 228-231. || doi: 10.5694/mja2.51673. Bariatric surgery: a call for greater access to coordinated surgical and specialist care in the public health system. Published online: 15 August 2022
O’Brien PE, Hindle A, Brennan L, et al. Long‐term outcomes after bariatric surgery: a systematic review and meta‐analysis of weight loss at 10 or more years for all bariatric procedures and a single‐centre review of 20‐year outcomes after adjustable gastric banding. Obes Surg 2019; 29: 3‐14.
Khorgami Z, Shoar S, Saber AA, et al. Outcomes of bariatric surgery versus medical management for type 2 diabetes mellitus: a meta‐analysis of randomized controlled trials. Obes Surg 2019; 29: 964‐974.
Kaul A, Sharma J. Impact of bariatric surgery on comorbidities. Surg Clin North Am 2011; 91: 1295‐1312.
Syn NL, Cummings DE, Wang LZ, et al. Association of metabolic–bariatric surgery with long‐term survival in adults with and without diabetes: a one‐stage meta‐analysis of matched cohort and prospective controlled studies with 174 772 participants. Lancet 2021; 397: 1830‐1841.
